Digital solutions like AI are becoming more and more common in healthcare, but the path to commercialization and a sustainable business is still fraught with peril.
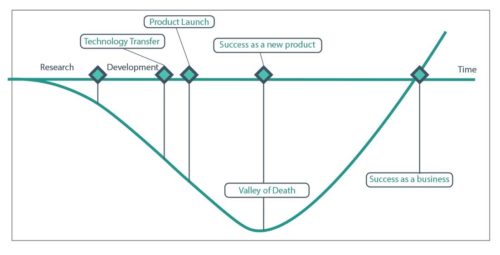
There is a lag in the healthcare system between getting technologies approved by the US Food and Drug Administration (FDA) and obtaining reimbursement from Centers for Medicare & Medicaid Services (CMS). Often CMS reimbursement valuation structures require significant clinical adoption of the technology to set reimbursement. This can stretch the gap from regulatory clearance with the FDA to reimbursement rate setting with CMS to five or more years.
For many technologies, not just AI, this creates a “Valley of Death” where innovation dies.
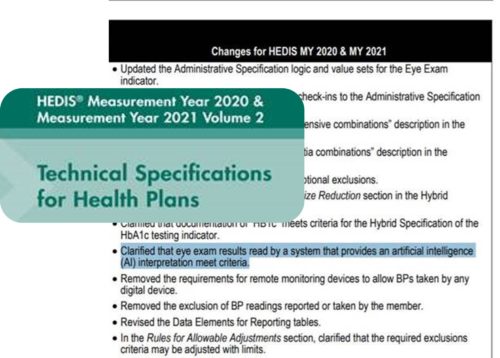
Even after crossing the “Valley of Death” technologies can still run afoul of legacy regulations that only contemplate the past. For example, language in HEDIS regulations for the diabetic eye exam specifically states a physician is needed as the required clinical decision. This requirement persists even after the FDA has validated an AI technology (LumineticsCore™ (formerly known as IDx-DR)) is a substitute to a physician driven test.
In 2020 the HEDIS measure language was updated to clarify that “results read by a system that provides an AI interpretation meet criteria,” showing industry progress toward full acceptance of autonomous AI. We appreciate the responsiveness of NCQA in making this change. We also think there is an opportunity to better link the regulatory clearance, reimbursement, and downstream impacts new technology has to legacy healthcare frameworks as we look to the future.
Is the healthcare system ready for AI?
A complete rework of the regulatory pathway to market within the healthcare system will likely take longer than stakeholders in technology, business, and innovation would like. That said, there have been some noteworthy changes made already worth celebrating.
- By working closely with the FDA to understand the requirements for autonomous AI in healthcare and closely following their guidance, the first ever DeNovo clearance for an autonomous AI in healthcare was granted to Digital Diagnostics for LumineticsCore (formerly known as IDx-DR)
- CMS was quick to see the benefits of bringing autonomous AI to healthcare and created the first ever autonomous AI Category I CPT code (92229)
- CMS further advanced the establishment of AI in healthcare when it set the first reimbursement rate for an AI CPT which was further validated by Medicare Administrative Contractors (MAC)
While the market is adopting the few already FDA cleared AI, there is still a learning curve for new innovators to understand how to get their AI through the process.
Ideally there would be a clearly stated “pathway to market” for AI regulatory clearance, reimbursement, and ultimately commercialization. Until that exists, Digital Diagnostics is working closely as a partner with other AI innovators to repeat the successful pathway our product, LumineticsCore (formerly known as IDx-DR), took to market. We invite those working on their own AI, with goals of making it autonomous, to reach out to us.
What should drive AI reimbursement?
At Digital Diagnostics we believe reimbursement for AI, and thus its commercial viability, should be based in the patient outcomes the technology drives. If an innovator manages to get reimbursement for a technology, but they are not driving better patient outcomes, there is still more work that needs to be done. A redesign of the product, or additional studies should follow, or the reimbursement should discontinue. The healthcare system applies this same logic to other healthcare innovations, and we think AI should be no exception.
If an AI simply increases a physician’s speed but doesn’t expand access and improve outcome by unburdening the physician to see more patients, that technology should be paid for by the physician, like how a practice might pay for their scheduling system. If we don’t differentiate between AI that drives patient outcome, and AI that automates other healthcare tasks, we are creating a perverse incentive. By doing so, we would be encouraging people to keep physicians in the loop merely to leverage existing Fee for Service (FFS) models, rather than focusing on Value Based Care (VBC).
Are patients ready for AI?
In most cases patients are not as concerned with whether a new technology is AI, so long as it is solving a problem that matters to them. The fact that a patient can now go to their local pharmacy and get a diabetic retinal exam with point-of-care results, and same day specialty appointments, matters more to them than what powers the device. It is not about the AI or the technology, it is about things like convenience, equity of access, and possible prevention of visual loss.
The mainstream media sensationalizes AI as if it will replace humans and fundamentally change the way we do healthcare. While AI is uniquely suited as a triage and automation tool, it is not meant to be a replacement for physicians or the human element of care. AI is not set up to eliminate care providers, but rather to offload repetitive narrow tasks with clear parameters, so providers can invest more time into their patients and help better manage holistic patient health.
Considerations for the future of AI
With continued development of highly validated AI systems that are built on an ethical foundation and strive to minimize bias while maximizing equity and access, AI in healthcare can not only be a commercial success but can have a positive impact on patient outcomes.
AI will continue to shift the focus toward what matters to the individual and enhance the emotional and educational aspects of care, allowing patients to take more ownership of their health and helping providers offer more accessible, convenient, and affordable care to address disparities and democratize healthcare.